If you suffer from asthma and take medication for it, then you likely already know what triggers an attack for you. Allergies and intensive exercise are common triggers for most people, but the good news is that both of these triggers can be managed – it just takes a bit of know-how and vigilance.
What Actually Causes Asthma In The First Place?
It’s very difficult to nail down exactly causes a person to become asthmatic, but doctors believe it could come down to genetic predisposition and under-exposure to allergens at an early age. Under-exposure would happen if a child is brought up in an overly clean and sterile home environment. You see moms, a bit of dirt isn’t so bad!
What Are The Most Common Asthma Triggers?
We spoke Hello Doctor’s resident GP, Dr Kotze, to find out what the most common asthma triggers are, and here’s her top list of triggers:
- Allergens such as dust mites, pollen, animal fur or feathers
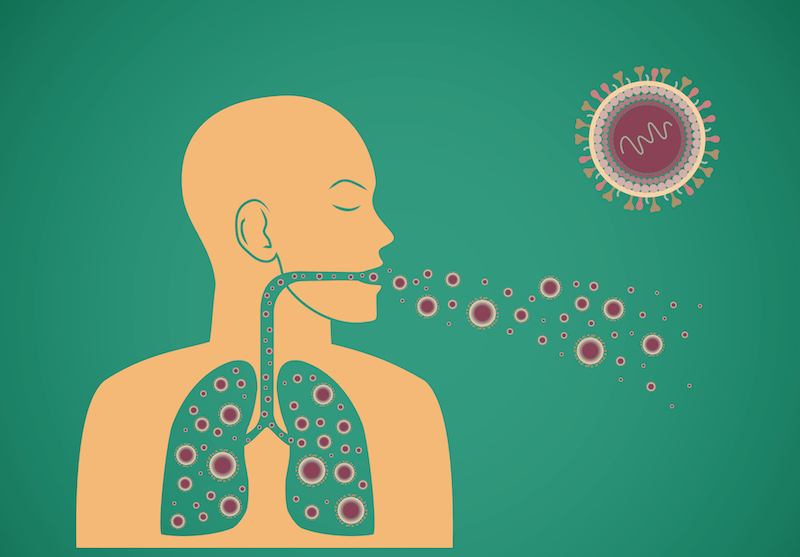
- Chest and airway infections, upper respiratory infections caused by cold and flu viruses, or sinus infections
- Airborne irritants: chemical fumes, cigarette smoke and pollution
- Medicines: non-steroidal anti-inflammatory painkillers including aspirin and ibuprofen
- Alcohol and foods containing sulphites: sulphites are used as preservatives in concentrated fruit juice, jam, prawns, certain wines, and processed or convenience meals
- Weather conditions: sudden changes in temperature, wind, poor air quality, cold and hot air, humidity
- Emotional factors: stress or laughing
- Living conditions: damp or mouldy walls, chemicals in carpets and flooring materials, and dust mites
- Intense exercise: some people find their asthma symptoms are worse when they exercise. This doesn’t mean you should avoid exercising, you just need to make sure you warm up slowly before you do start exercising, to help prevent an attack
- Severe heartburn
How Do I Stay Healthy With Asthma?
Asthma affects people of all ages, young and old, and the chances are your asthma started when you were still young. When it comes to staying healthy, the most important thing you can do is to know what triggers your asthma, and how you can control it. If you’re able to do this, you should be able to reduce symptoms and the number of attacks you have.
Make sure you have regular check-ups – at least twice a year – with your doctor, to help ensure your asthma is under control and that you’re taking the right medication. It’s very important that you know how to use your inhaler correctly, and that your close friends and family also know how to use it in case of an emergency. Always carry your inhaler with you!