It may not be the most pleasant topic, but understanding your bowel movements better can improve your health, and even save your life! Your stools hold secrets and valuable clues to your health, through their texture, shape and smell. The ideal poop should be soft and easy to pass; not hard, dry or overly loose.
According to Dr Danie Pauw from Health24, one to three times per day is considered normal for some people, while others only go a few times a week. But it shouldn’t be less than three times a week.
What is poo and why should you pass it?
About half of your faeces are made of water. The rest is undigested solids, dead and live bacteria, mucous and fat. Through your poo you also get rid of unwanted metabolic waste products and toxins. It’s an important way for your body to eliminate what it no longer needs. That funky smell isn’t bad either; it’s a good sign.
Dr Ken Heaton of the University of Bristol in the UK created a charted that classifies the different forms of human faeces. The chart was first published in the Scandinavian Journal of Gastroenterology in 1997.
Type 1: Is hard to pass; comes out in separate hard lumps, like nuts.
You need to drink more water and eat more fruit and vegetables.
Type 2: Lumpy and sausage-shaped.
You need to load up on fluids and fibre!
Type 3: Looks like sausage with cracks on its surface.
This is relatively normal, but your cracks indicate that you could do with more water.
Type 4: Is a snake- or sausage-shaped; smooth and long.
This is the best poop! You’re doing just fine.
Type 5: Soft blobs with clear cut edges.
This is pretty normal.
Type 6: A mushy stool; with fluffy ragged pieces.
Your poop is on its way to becoming diarrhoea.
Type 7: Entirely liquid! Your poo has no solid pieces and is watery.
Diarrhoea!
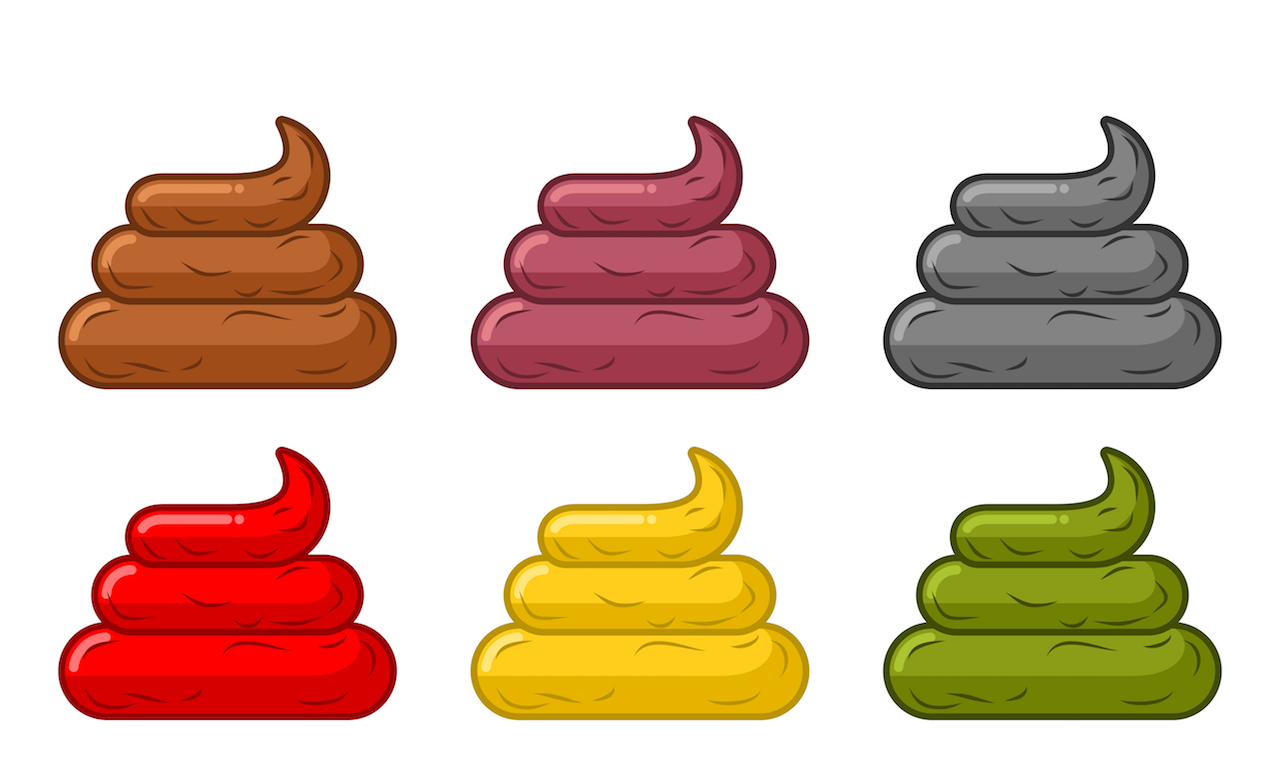
The colour and smell of your poop matters too:
- A healthy poop will have a foul odour but shouldn’t smell too strong; it should be mild and pass quickly. A potent smell could be a sign of a medical condition.
- Black or red: A sign of potential bleeding in the upper gastrointestinal tract. Certain foods like liquorice could be the cause.
- Green: You may be eating a lot of leafy greens and vegetables that turn your stools green. Or there’s bile pigment in the stool because of diarrhoea.
- Yellow: Too much fat in your stool, or it’s a celiac disease; a disorder where your body doesn’t absorb nutrients well.
- Pale, white or clay-coloured: This is caused by a lack of bile. People with liver and gallbladder problems may find this common.
- Orange: This is caused by a compound found in vegetables, fruit and grains. Blocked bile ducts can also lead to orange stools.
Pooping 101
Research finds that squatting is better for your gut than sitting down. When you squat, you can pass stools completely and more naturally without straining. Also, your stools needs to sink. Floating stools are an indication of high fat content which can be a sign of malabsorption, a condition where you can’t absorb fat and other nutrients.
If you are worried about your stools, why not speak to one of our doctors? It’s best to pick up any underlying conditions before it gets too serious.
References:
- https://articles.mercola.com/sites/articles/archive/2016/07/23/healthy-stool.aspx
- http://www.foodmatters.com/article/what-your-poop-says-about-your-health
- https://startsat60.com/health/everyday-health/gut-health/what-does-your-poo-say-about-you
- https://wellnessmama.com/7013/squatty-potty/
- https://www.healthline.com/health/digestive-health/types-of-poop#length-of-time
- https://www.medicinenet.com/stool_color_changes/article.htm
- https://www.thealternativedaily.com/what-the-smell-of-your-poop-means/