Tuberculosis (TB) is a disease caused by bacteria that spreads from person to person through the air. When people with lung TB cough, sneeze or spit, they spread the TB germs into the air. Inhaling only a few of these germs can cause an infection in another person.
Having a strong and healthy immune system can prevent you from becoming sick.
There are two types of TB:
1. Latent TB: Also called inactive TB. This isn’t contagious. The bacteria remains in your body in an inactive state and causes no symptoms. Treatment is important if you have latent TB to help control the spread of the disease, as it can turn into active TB.
2. Active TB: This type makes you sick, and in most cases can spread to others. It can develop either in the first few weeks after being infected with the TB bacteria, or many years later.
Signs and symptoms of active TB include:
- A cough that lasts three or more weeks
- Coughing up blood
- Chest pain, or pain with breathing or coughing
- Unintentional weight loss
- Fatigue
- Fever
- Night sweats
- Chills
- Loss of appetite
TB can also affect other parts of your body, including your kidneys, spine or brain. When it develops outside your lungs, signs and symptoms differ according to the organs involved.
For instance, TB of the spine may give you back pain, and TB in your kidneys might cause blood in your urine.
Tests used to screen for TB:
There’s no single test that can be used to test for TB in all circumstances.
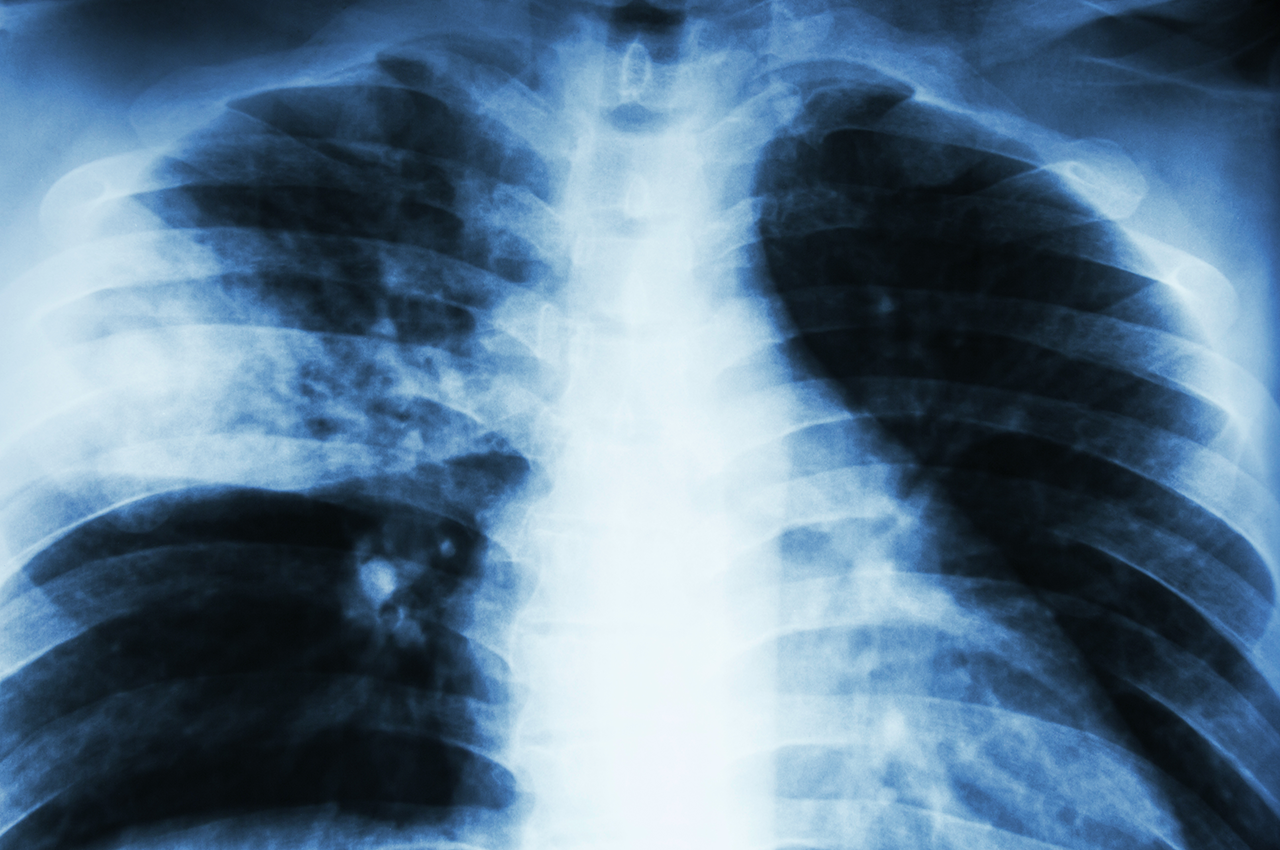
1. A chest X-ray (best used to screen for active TB) is taken to look for changes in the lungs that could show signs of active TB or scars from a previous TB infection.
2. A tuberculin skin test is done by injecting a solution containing a protein made from tuberculosis bacteria just under the top layer of skin on the forearm. If after 48-72 hours the skin at the injection site develops a raised red bump, it indicates that you may be infected with TB.
If a skin test is positive, doctors will consider your risk factors and order additional testing to determine the best course of treatment. For this reason, doctors don’t rely on the skin test alone to confirm a diagnosis.
3. Blood tests may be ordered on their own or after a positive skin test. The different blood tests offer ways to measure the body’s immune response to the presence of bacteria.
4. Imaging tests
If you’ve had a positive skin test, your doctor will likely order a chest X-ray or a CT scan. This may show changes in your lungs caused by active tuberculosis. CT scans provide more-detailed images than X-rays do.
5. Sputum tests
If your chest X-ray shows signs of TB, your doctor may take samples of the mucus that comes up when you cough. The samples are tested for TB bacteria.
Sputum samples can also be used to test for drug-resistant strains of TB. This helps your doctor choose the medications that are most likely to work. These tests can take four to eight weeks to be completed.
Treatment
TB treatment takes much longer than treating other types of bacterial infections.
For active tuberculosis, you must take antibiotics for at least six to nine months. The types of medications and duration of treatment will depend on your age, health, possible drug resistance and the infection’s location in the body.
Preparing for your appointment
If you suspect that you have TB, see a doctor. At the time you make the appointment, be sure to ask if there’s anything you need to do in advance. In addition,
- Write down any symptoms you’re experiencing
- Write down key personal information; include any recent life changes or international travel.
- Make a list of all medications, vitamins or supplements you’re taking.
- Write down questions to ask your doctor.
Some basic questions to ask your doctor include:
- What’s the most likely cause of my symptoms?
- Do I need any tests?
- What treatments are available? Which do you recommend?
- What if the treatment doesn’t work?
- How long do I have to stay on the treatment?
- How often do I need to follow up with you?
- I have other health problems. How can I manage these conditions together?