The single largest infectious killer of humans for centuries is a curable disease – and we have the potential to put an end to unnecessary deaths. It all starts with knowledge.
Do you know what the leading cause of death in South Africa is? It may surprise you to learn that it is a treatable disease. Tuberculosis, commonly called TB, takes far too many lives every year. What’s worse, numbers are still climbing. For a condition that can be successfully cured, this is unacceptable.
So how can we beat TB? The answer lies in getting diagnosed and treated – for that to happen, we need to fight the stigma. TB Awareness Month aims to do just that.
Stop the stigma to win the war
Because TB often occurs along with HIV/AIDS, sufferers can be reluctant to share their diagnosis. There’s also the stigma of contributing factors like overcrowding, malnutrition, and alcohol and drug abuse. Yes, these do play a role, but anyone, anywhere, from all walks of life can get TB. In fact, an estimated 80% of people in SA have been infected with the bacterium that causes TB. There can be no shame when the majority of people you know already carry TB.
But it’s human nature to want to hide from bad news – we just can’t face what diagnosis might mean so we avoid finding out. People are also afraid of the stories about TB medication side effects. But the reality is that TB will not go away by simply pretending that it doesn’t exist – this only makes things worse.
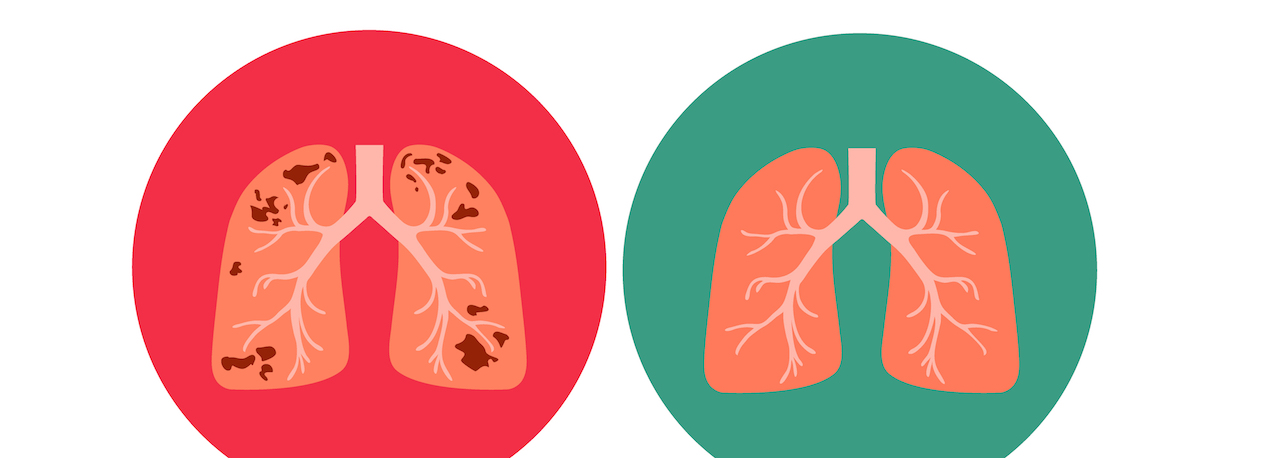
The good news is that TB can be treated by following the prescribed course of treatment. The bad news is that we cannot treat what we don’t know is there, which is why putting aside fears and stigmas to get tested is crucial… the sooner, the better.
Steps to tackle TB
- Know your status
The World Health Organisation estimates that 40% of people infected with TB don’t get diagnosed. Without diagnosis, they’ll never get the help they need. TB tests are quick and, in SA, they’re free at government clinics. Two sputum (spit) samples are taken and results are available within a few days. - Look after yourself
Give yourself a fighting chance of beating any bugs and, if you do get sick, of recovering more quickly. A balanced diet with fruits, vegetables, protein and wholegrains is crucial. Daily exercise, particularly in the fresh air, helps to keep your body healthy and combats stress, which also affects the immune system. And, of course, steer clear of smoking and alcohol. - Vaccinate your children
The BCG vaccine against TB is crucial for children as they’re at a higher risk, both of contracting TB and of developing severe forms, such as deadly TB meningitis or TB affecting organs besides the lungs. The vaccine is generally not given to adults as it’s less effective than when given to children. - Be considerate
Remember the lessons we learnt from COVID-19? When coughing or sneezing, cover your mouth and nose with your arm or a tissue, don’t spit and keep your distance from others. If you’ve been diagnosed, be courageous by telling those you’ve interacted with so they can be tested too. - Complete your treatment
If you’re diagnosed with TB, you’ll be prescribed a course of medication that lasts at least six months. It is true that the treatment can have side effects but, fortunately, new breakthroughs are set to improve this. What’s more, after just two weeks on treatment, most people are already no longer infectious, so you can stop the spread. Because it takes longer to completely rid yourself of TB, it’s vital to complete the full treatment. Sticking to your treatment programme is truly the most powerful thing you can do to help yourself and everyone around you.
TB has been with us for thousands of years. But, today, with unprecedented access to information, new treatment programmes and fast, painless testing, we’re in the best position ever to overcome it. By working together, we can end TB – once and for all.
Where to find help online
- For information and education about TB: TB Proof
- For advice, information and resources on TB and HIV: TB/HIV Care Association
- Join the Tuberculosis Support Group – South Africa on Facebook or ask your local clinic for support group referrals.