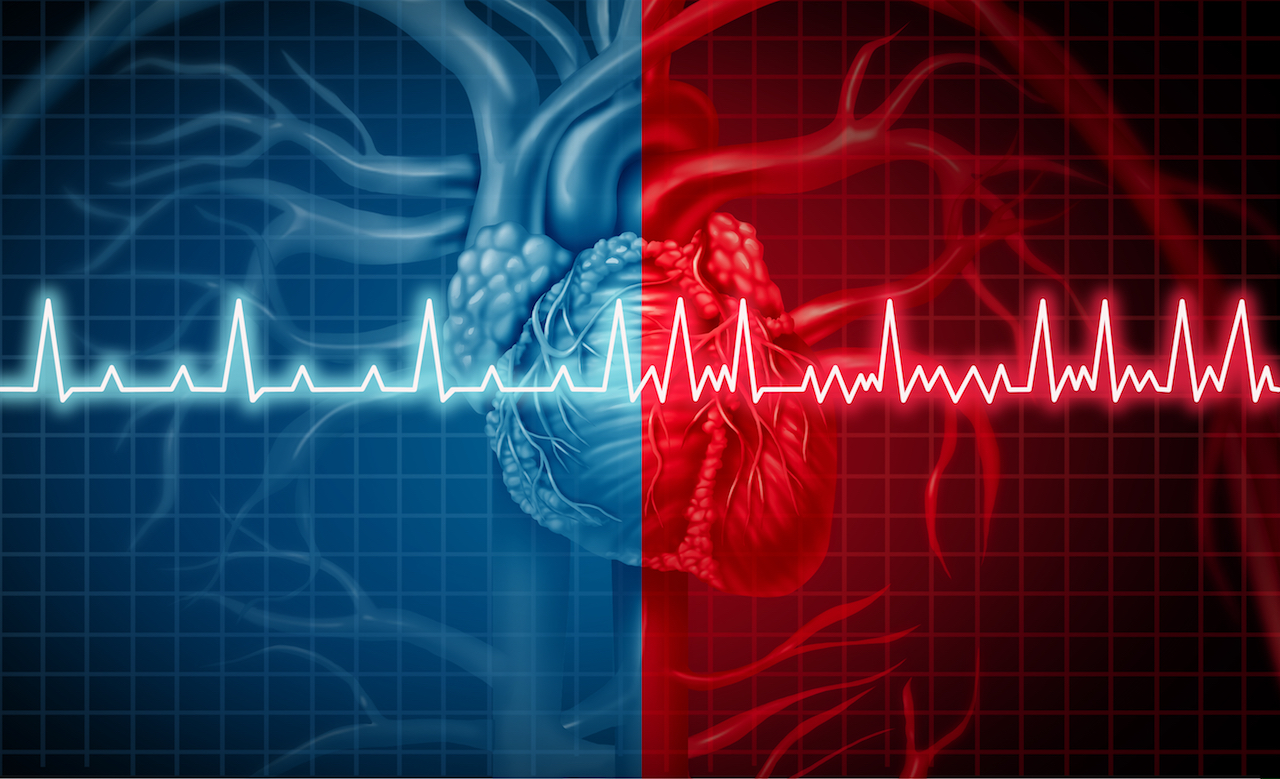
Heart rate variability refers to differences in time between each heartbeat. For example, if your heart rate is 60 beats per minute, it’s not necessarily beating once every second. Within that minute there may be 0.9 seconds between two beats, and 1.15 seconds between two others. The greater this variability is, the more “prepared” your body is to perform at an optimal level.
Heart rate vs. heart rate variability?
Heart rate (HR)
Heart rate is measured in beats per minute and refers to the average number of the beats in a given time period.
For example, a 60 beats per minute HR could mean 1 beat per second or it could mean an average of 1 beat every 0.5s, 1.5s, 0.5s, 1.5s, etc.
Generally, a low HR is measured during rest, while a high HR is associated with movement, exercise and sometimes stress.
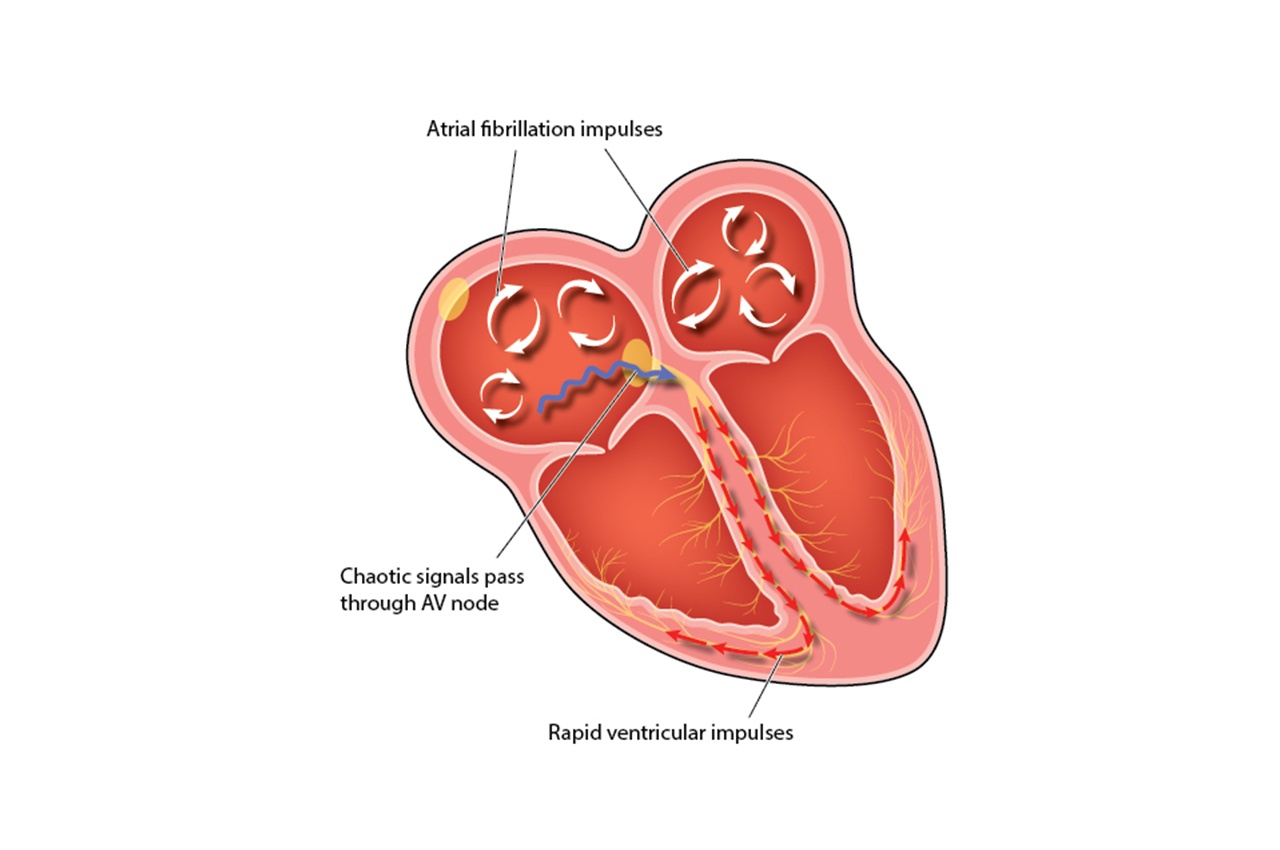
Heart rate variability (HRV), on the other hand, measures the specific changes in time between consecutive heartbeats.
The time between beats is measured in milliseconds (ms) and is called an “R-R interval” or “inter-beat interval (IBI).
Why should you check heart rate variability?
Checking your heart rate variability is a great way to identify how well your autonomic nervous system is functioning.
When you’re in a fight-or-flight mode, or feeling very stressed, the variation between heartbeats is usually low. But if you’re in a more relaxed state, the variation between beats is higher.
The healthier the autonomic nervous system, the faster you’re able to switch mechanisms, showing more resilience and flexibility, especially to stress. A higher HRV is associated with improved cardiovascular fitness and resilience to stress, whereas a low HRV has been linked to anxiety, heart disease and an increased risk of early death.
Your HRV may also help give an idea of your lifestyle habits. Your HRV changes as you incorporate exercise, mindfulness, meditation and sleep into your life. This is a great way to not only track how your nervous system reacts to the environment, but also to your emotions, thoughts, and feelings.
How to improve heart rate variability
Stay hydrated: The more hydrated you are, the easier it is for your blood to circulate and carry oxygen and nutrients to your body.
Avoid alcohol: One night of drinking may negatively affect your HRV for up to five days.
Eat clean: Poor nutrition has a negative effect on HRV
Quality sleep: The quality and consistency of your sleep is important. Going to bed and waking up at similar times every day is beneficial.
Auto-regulation: Adopting a consistent schedule for your body especially with sleep and eating is helpful. Your body operates more efficiently when it knows what’s coming.