Meet Harnaam Kaur: a 26-year old body positivity campaigner and model, and Guinness World Record holder for being the youngest woman to have a full beard. After years of struggling to keep her facial hair under control, she has decided to grow them into a full beard, and now campaigns for women to be positive, and accept their bodies as they are.
The reason for her stubble? She has polycystic ovarian syndrome (PCOS).
What is PCOS?
PCOS is a hormonal disorder in which your sex hormones; oestrogen and progesterone are out of balance. This imbalance causes the growth of ovarian cysts (benign masses on the ovaries), which can affect your menstrual cycle, fertility and appearance.
Symptoms
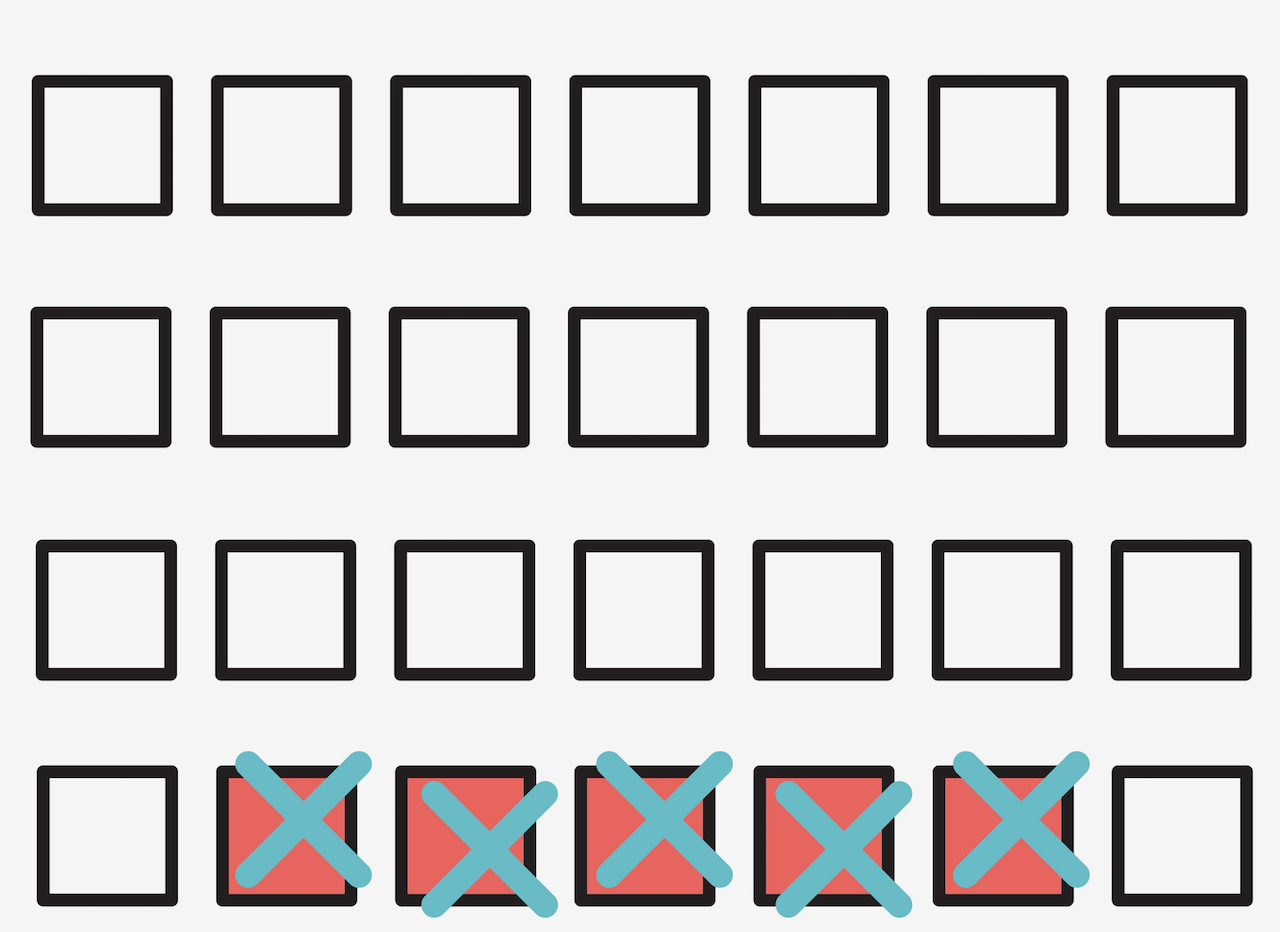
PCOS symptoms usually start soon after your first menstrual period. They tend to be mild at first, and develop gradually. You may only have a few symptoms or a range of them.
The type and severity varies from woman to woman. Symptoms are typically more severe if you’re overweight or obese.
Watch for
- Irregular periods or no periods.
- Excessive hair growth (hirsutism) on the face, chest, back, belly, or buttocks.
- Rapid weight gain and trouble losing weight.
- Oily skin.
- Acne.
- Pelvic pain.
- Hair loss on the scalp.
- Difficulty getting pregnant. PCOS is a leading cause of infertility in women.
- Mood swings.
- Depression.
What is the cause?
The exact cause of PCOS is unknown, but research suggests that it runs in families. If your mother or sister has PCOS, you’re at a higher risk than normal.
Overproduction of the hormone, androgen may factor into PCOS. Androgen is a male sex hormone that women also produce. If you have PCOS, your body may produce abnormally high levels of androgen. This can affect the development and release of eggs during ovulation, and lead to hirsutism and acne.
Excess insulin is another contributing factor. Insulin is the hormone that helps convert sugars and starches into energy. If you have PCOS, your body is unresponsive to the action of insulin. When your body has a problem using insulin, your blood sugar levels go up, and you produce more insulin. High levels of insulin can cause your body to produce more androgen. This can lead to ovulation problems, weight gain, irregular periods, and infertility.
How it is diagnosed
There’s no definitive test to diagnose PCOS. To make a diagnosis, your doctor will review your medical history, symptoms and menstrual cycle.
He’ll then do a physical exam to look for signs of PCOS like extra body hair and acne. He’ll check your height and weight to see if you have a healthy body mass index (BMI).
Your doctor may perform:
- A pelvic exam to inspect your reproductive organs for masses, growths or other abnormalities.
- An ultrasound to check for cysts on your ovaries.
- A blood test to measure your hormone levels, blood sugar, and cholesterol. This can help rule out other conditions that mimic the symptoms of PCOS.
Treating PCOS
PCOS can’t be cured, but the symptoms can be managed.
Your doctor may prescribe:
- Birth control pills to decrease androgen production and regulate oestrogen. This can regulate your periods, treat acne, and reduce excess hair growth.
- Fertility medication to help you ovulate.
- Diabetes medication to lower your insulin levels, and improve the way your body uses insulin. These meds can also slow the progression of diabetes and boost weight loss.
- Ovarian drilling to reduce androgen levels and help stimulate ovulation. Your doctor may puncture your ovary with a small needle that carries an electric current. The part of the ovary that’s producing androgens will then be destroyed.
In the long run, you will need to stick to a healthy diet, get lots of regular exercise, and lose the extra weight to manage the symptoms of PCOS and prevent long-term complications. Losing even a modest amount of weight can help balance your hormones, lower your blood sugar levels, and restore normal menstrual patterns and ovulation. It can also increase the effectiveness of your PCOS medications.
To get rid of excess hair, your doctor may recommend an eflornithine cream to slow hair growth. Electrolysis is another option. This method uses a needle to emit a pulse of electric current to damage and destroy each hair follicle. You can also get rid of unwanted hair with shaving, plucking, waxing or with depilatories (creams that dissolve hair).
Or, you can follow the brave footsteps of Harnaam Kaur, and rock a beard. Who says you can’t?!
References
- http://metro.co.uk/2017/08/01/bearded-lady-and-proud-bullies-told-me-to-die-because-of-my-pcos-but-now-i-love-my-look-6808201/
- http://www.webmd.com/women/tc/polycystic-ovary-syndrome-pcos-topic-overview#1
- http://www.healthline.com/health/polycystic-ovary-disease#symptoms3
- http://www.mayoclinic.org/diseases-conditions/pcos/symptoms-causes/dxc-20342150