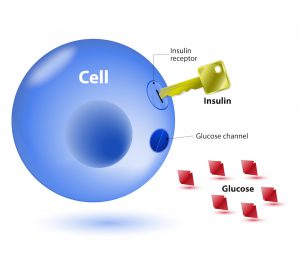
According to the American Heart Association, diabetics are two to four times more likely than people without diabetes to die of heart disease or experience a life-threatening stroke.
What’s more, those who don’t control their condition efficiently have an increased chance of developing cardiovascular conditions, nerve damage and kidney disease.
Fortunately, you can eat your way to better health by munching on plenty of fresh vegetables. Veggies are not only chockful of fibre, and nutrients, the non-starchy varieties like baby corn, asparagus and bean sprouts are low in carbohydrates.
The best foods for diabetics are low-carb, low-sugar and high in fibre. This also includes digestion-slowing macronutrients like healthy fats and protein.
Here are some vegetables that diabetics must include in their diet:
Dark green leafy vegetables
Kale, spinach and collards are dark green leafy vegetables chockful of vitamins and minerals like vitamins A, C, E, and K, iron, calcium and potassium.
Spinach is particularly rich in vitamin K, along with minerals like magnesium, folate, phosphorus, potassium, and zinc. These veggies are low in calories and carbohydrates too. Add dark leafy vegetables to salads, soups and stews.
Sweet potatoes
A starchy vegetable packed with vitamin A and fibre, sweet potatoes are also a good source of vitamin C and potassium. If you find yourself craving something sweet, replace regular potatoes with sweet potatoes and sprinkle cinnamon on top.
Beans
Beans offer a combination of plant protein and soluble fibre that can help boost feelings of fullness and manage blood sugar levels. They can also reduce the risk of coronary heart disease.
Peppers
All shades of peppers offer fibre, folate, vitamin K, beta carotene and a range of minerals.
They’re packed with vitamins A and C. A cup of chopped red, yellow or orange peppers can provide more than 100% of the recommended daily value for both vitamins.
Raw peppers can be a perfect snack on their own or are also good dipped in salsa, hummus, guacamole or a yoghurt dip.
Broccoli and cauliflower
Cruciferous veggies like broccoli and cauliflower are diabetes-friendly food that have a compound called sulforaphane. This compound triggers anti-inflammatory processes that improve blood sugar control and protect blood vessels from the cardiovascular damage that’s often a consequence of diabetes.
Sulforaphane also helps change the body’s natural detox mechanisms – it influences enzymes to turn dangerous cancer-causing chemicals into more innocent forms that the body can easily release.
References:
- https://www.medicalnewstoday.com/articles/317225.php
- https://www.eatthis.com/best-foods-diabetes/
- https://www.everydayhealth.com/hs/managing-type-2-diabetes/best-and-worst-foods/
- https://healthyeating.sfgate.com/can-diabetics-eat-peppers-10557.html
- https://www.thehealthy.com/diabetes/type-2-diabetes/10-diabetes-super-foods/