Could stress really prevent you from getting pregnant?
Stress is often described as an event that a person sees or feels as threatening to their life. So, the body responds with a “fight or flight” response in order to protect itself.
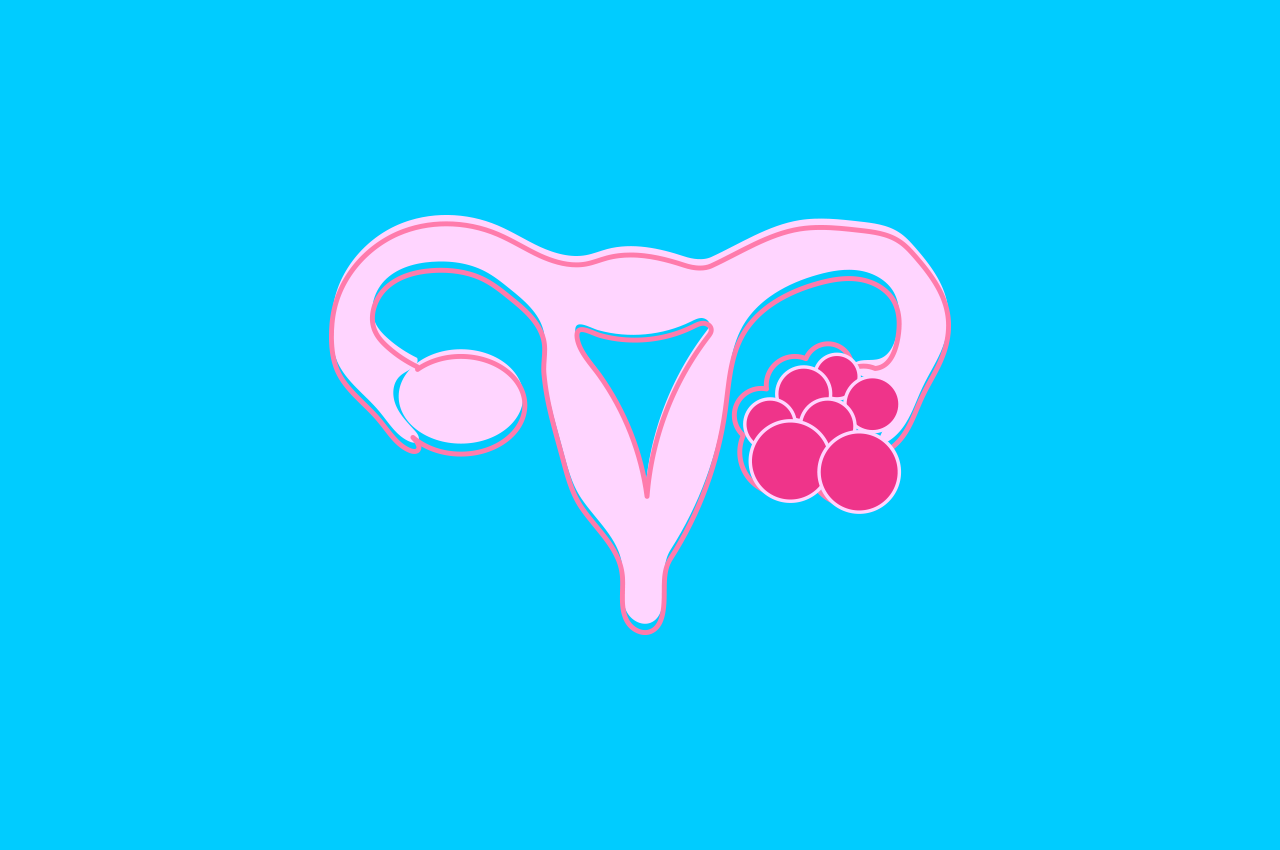
According to research on the relationship between stress and infertility, the cause of infertility isn’t always clear. There may be a basic health condition like polycystic ovarian syndrome (PCOS), endometriosis, male infertility, or the frustrating diagnosis of unexplained infertility.
Stress, depression and anxiety are described as common consequences of infertility.
Stress and your behaviour
While stress alone doesn’t necessarily cause infertility, it can push a person toward unhealthy behaviours. These unhealthy behaviours can affect your fertility.
We all resort to unwholesome patterns or routines when stressed. But the following habits can actually affect your fertility:
- Binge eating, emotional eating or not eating enough.
- Sleeping too much or too little.
- Not exercising enough or pushing yourself to overdo it.
- Drinking too much alcohol.
- Smoking.
- Drinking too much caffeine, especially if you’re sleep-deprived.
- Loss of interest in sex with your partner.
Infertility and stress
Stress can affect the gland in the brain that manages your emotions, appetite and the hormones that tell your ovaries to release eggs. When you’re stressed out, you may ovulate later in your cycle or not at all. So, if you’re only having sex around day 14, thinking that you’re about to ovulate, you may miss your opportunity to conceive.
Research has shown that people who get less than five hours of sleep each night are more likely to suffer from obesity, and obesity can lead to problems with fertility.
Don’t let stress get in the way
Reducing stress is good for your health, and may improve your chances of falling pregnant. Finding ways to keep stress in check by developing better coping strategies to help you feel more in control and improve your overall wellbeing.
Improve emotional health
Try these:
- Acupuncture.
- Aerobic exercise (may be reduced during treatment).
- Journaling.
- Listening to music.
- Massage therapy.
- Meditation.
- Mind-body groups.
- Mindfulness.
- Progressive muscle relaxation.
- Psychotherapy and cognitive behavioural therapy.
- Self-help books.
- Support/educational groups.
- Walking/hiking.
- Yoga.
References:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6016043/
- https://www.verywellfamily.com/can-stress-keep-you-from-getting-pregnant-1959951
- https://www.babycenter.com/404_can-stress-get-in-the-way-of-getting-pregnant_1336350.bc
- https://www.reproductivefacts.org/news-and-publications/patient-fact-sheets-and-booklets/documents/fact-sheets-and-info-booklets/stress-and-infertility/