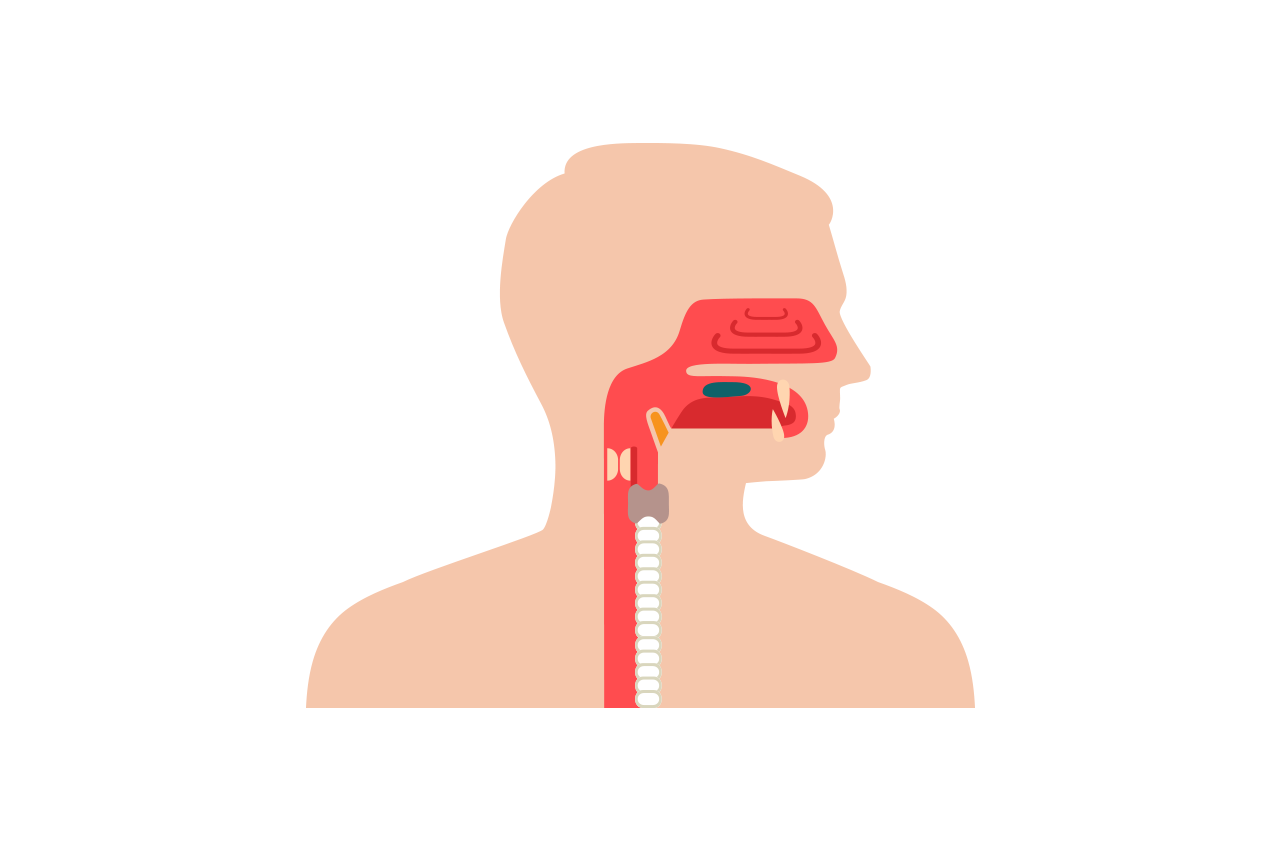
Do you feel as if your throat is stuck and you can’t swallow? You may have dysphagia, a difficulty in swallowing.
Types of dysphagia
Oropharyngeal dysphagia is when you cannot swallow, while oesophageal dysphagia is having difficulty passing food down your throat. You feel as though food or drink has become stuck in your throat or chest.
Oesophageal dysphagia
- This type of dysphagia is caused by:
- Muscles in your throat not relaxing properly to let food into your stomach.
- Abnormal spasms in your throat muscles.
- A narrow throat from scar tissue or a tumour. Scar tissue can stiffen your lower throat muscles.
- Food or other objects stuck in your throat. Those with dentures or who have difficulty chewing are more at risk for this.
- A narrowing of your lower throat.
- Damage to your throat tissue from stomach acid backing up into it (reflux).
- Radiation treatment for cancer which causes swelling or scarring of your throat.
Oropharyngeal dysphagia
This type of dysphagia is caused by conditions like a stroke, head and neck cancer, head, neck or spinal surgery, or from abnormalities or injuries to your spine.
Other causes include:
- A small pouch developing and catching food just above your throat.
- Multiple sclerosis, muscular dystrophy and Parkinson’s disease.
- Cancer and radiation treatment for cancer.
- Ageing.
- Persistent infections.
Symptoms
You may have dysphagia if you:
- Feel pain when you swallow.
- Cannot swallow.
- Cough or choke during meals.
- Bring up food or stomach acid.
- Feel like food is stuck in your chest.
- Experience constant drooling.
- Have difficulty chewing.
- Have a hoarse or wet sounding voice when you eat.
- Have heartburn.
- Experience sudden weight loss.
Diagnosis and treatment of dysphagia
Dysphagia can have serious complications: weight loss and dehydration; malnutrition; pneumonia from breathing in food, and fatal choking. Treatment is wide-ranging and will depend on what is causing the problem,.
The “gold standard” for diagnosis of oropharyngeal dysphagia is a fibre optic endoscopy, where a tube with a light at the end is inserted in your throat.
There are other methods: X-rays, CT and MRI scans, and physical examinations of your throat. Your doctor may also ask you to drink or eat foods and liquids that show up under X-rays so he can watch your throat as you swallow. He will look for a lack of coordination in your muscles. They may also use a pressure recorder to assess the strength of the muscles in your throat.
Once your condition has been diagnosed, a speech or swallowing therapist can teach you exercises to coordinate your swallowing muscles or get the nerves that cause your swallowing reflex back in action.
You may also learn swallowing techniques, This type of therapy can help with long term management of the condition.
Treatment for oesophageal dysphagia includes:
- Dilation, where your doctor may insert a medical balloon or flexible tubes to stretch and expand the width of your throat.
- Surgery to remove any tumours or fix any abnormalities to clear your throat.
- Medications to reduce stomach acid. Your doctor may also prescribe muscle relaxants or corticosteroids depending on whether spasming muscles or inflammation is causing your dysphagia.
- A liquid diet or feeding tube for severe dysphagia.
- Surgery to put in a stent – a metal or plastic tube that holds your throat open to help food pass smoothly.
While dysphagia itself cannot be prevented, by eating and chewing slowly, and managing other conditions, such as reflux you can lower your risk of experiencing occasional swallowing difficulties.